How to diagnose asthma in children
Take a structured clinical history. Consider if low, moderate or high suspicion of asthma.
Specifically check for:
- Wheeze, cough or breathlessness
- Daily or seasonal variation in these symptoms
- Any triggers that make symptoms worse
- A personal or family history of atopic disorders
- Food allergies
- Comorbidities, including rhinitis, chronic rhinosinusitis, acid reflux, obesity, obstructive sleep apnoea, anxiety
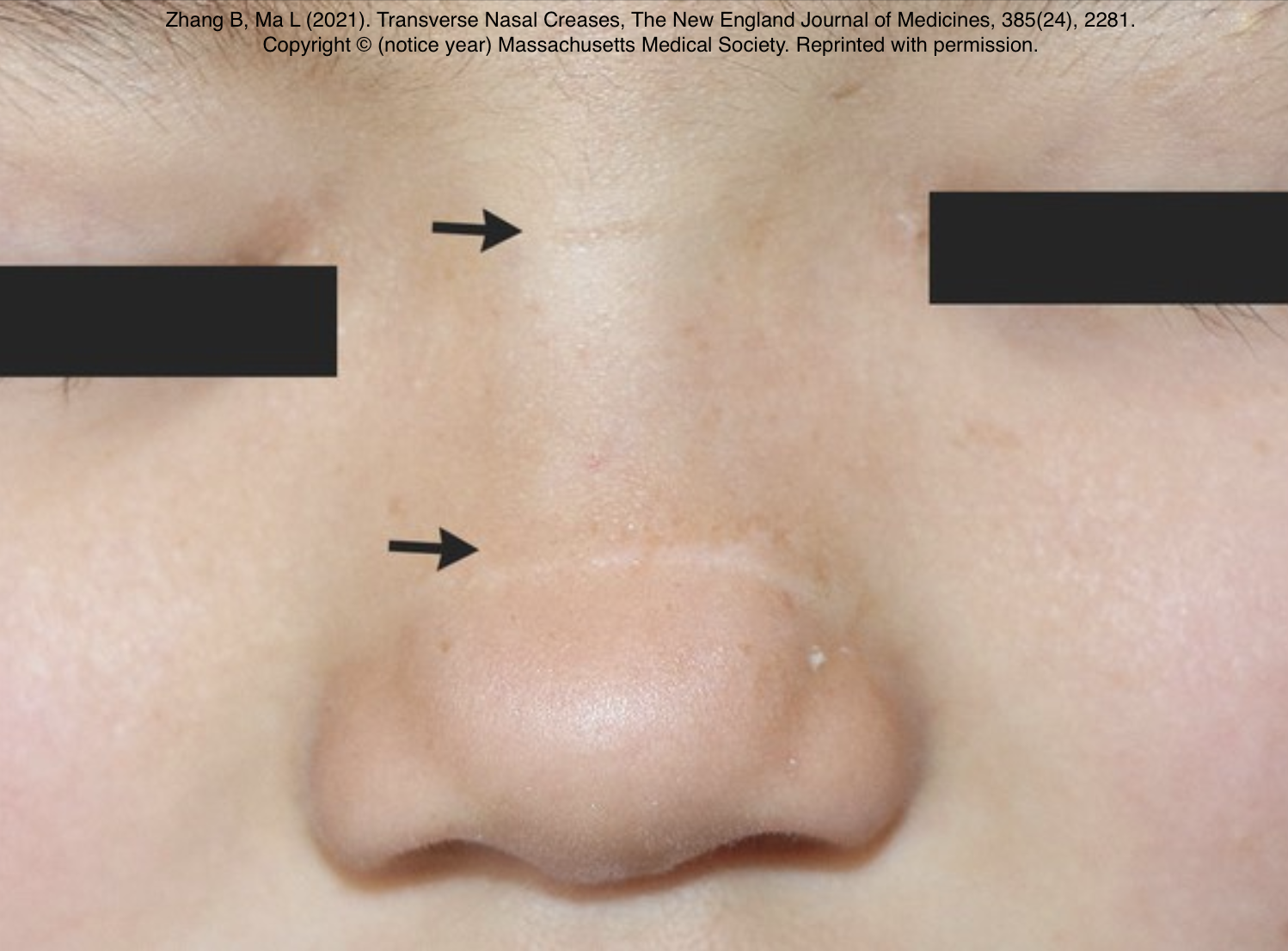
Examine to identify expiratory polyphonic wheeze and signs of other causes or respiratory symptoms. Remember asthmatics can have a normal examination when well. Observe for other signs including hyper-inflated chest, eczema and transverse nasal crease.
Suspected asthma under 5 years
Treat symptoms based on observation and clinical judgement, and review the child on a regular basis.
Consider a trial of twice daily paediatric low-dose moderate dose Inhaled Corticosteroids (ICS) for 8 weeks for children under 5 with suspected asthma and:
- Symptoms at presentation that indicate the need for maintenance therapy (for example, interval symptoms in children with another atopic disorder), or
- Severe acute episodes of difficulty breathing and wheeze (for example, requiring hospital admission, or needing 2 or more courses of oral corticosteroids).
If symptoms do not resolve during the trial period, take the following sequential steps:
- Check inhaler technique and adherence.
- Check whether there is an environmental source of their symptoms (for example mould in the home, cold housing, smokers or indoor air pollution).
- Review whether an alternative diagnosis is likely.
If none of these explain the failure to respond to treatment, refer the child to a specialist in asthma care.
Consider stopping ICS and SABA treatment after 8 to 12 weeks if symptoms are resolved. Review the symptoms after a further 3 months.
If symptoms resolve during the trial period, but then:
- Symptoms recur by the 3 month review, or
- The child has an acute episode requiring systemic corticosteroids or hospitalisation, restart regular ICS (begin at a paediatric low dose and titrate up to a paediatric moderate dose if needed) with Short Acting Beta Agonist (SABA) as needed and consider a further trial without treatment after reviewing the child within 12 months.
If suspected asthma is uncontrolled in children under 5 on a paediatric moderate dose of ICS as maintenance therapy (with SABA as needed), consider Montelukast 4mgs in addition to the ICS. Give the LTRA for a trial period of 8 to 12 weeks (unless there are side effects), then stop if it is ineffective.
If suspected asthma is uncontrolled in children under 5 on a paediatric moderate dose of ICS as maintenance therapy, and a trial of an LTRA has been unsuccessful or not tolerated, stop the LTRA and refer the child to a specialist in asthma care for further investigation and management.
If they still have symptoms when they reach 5 years, attempt objective tests.
If a child is unable to perform objective tests when they are aged 5:
- Try doing the tests again every 6 to 12 months until satisfactory results are obtained.
- Refer for specialist assessment if the child's asthma is not responding to treatment.
- Refer to a specialist respiratory paediatrician any preschool child with an admission to hospital, or 2 or more admissions to an emergency department, with wheeze in a 12 month period.
Suspected asthma 5 to 16 years
Consider objective testing, following algorithm below.
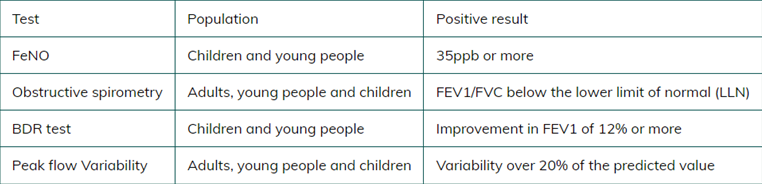
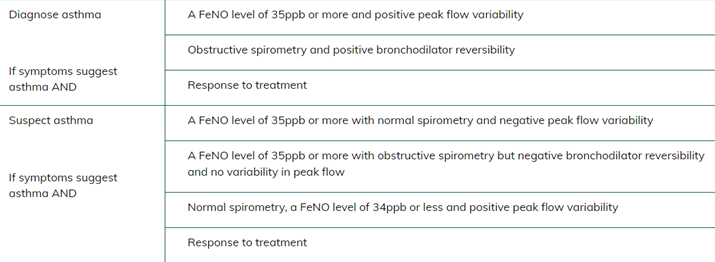
Lung function tests for children over 5 years
Measure the Fractional Exhaled Nitric Oxide (FeNO) level in children with a history suggestive of asthma. Diagnose asthma if the FeNO level is 35 ppb or more.
If the FeNO level is not raised, or if FeNO testing is not available, measure BDR with spirometry. Diagnose asthma if the FEV1 increase is 12% or more from baseline (or if the FEV1 increase is 10% or more of the predicted normal FEV1).
If spirometry is not available or it is delayed, measure PEF twice daily for 2 weeks. Diagnose asthma if PEF variability (expressed as amplitude percentage mean) is 20% or more.
To calculate PEFR variability using the daily amplitude percent mean method, you work out the variability for each day and then use that to find the average over the recording period.
- Daily variability = Difference between highest and lowest peak flows / Average of highest and lowest.
- Formula to calculate peak flow variability for each day: [(Highest - Lowest) / (Highest + Lowest) / 2] x 100 = Percentage variability.
- Overall variability = Total of daily variabilities / Number of days.
- Regard a value of more than 20% variability overall variability as a positive test.
PEF charting when asthma is well controlled is unlikely to confirm variability.
For further explanation and information about peak flow please visit PCRS peak flow consensus.
If asthma is not confirmed by FeNO, BDR or PEF variability but still suspected on clinical grounds, either perform skin prick testing to house dust mite or measure total IgE level and blood eosinophil count.
Exclude asthma if there is no evidence of sensitisation to house dust mite on skin prick testing or if the total serum IgE is not raised.
Diagnose asthma if there is evidence of sensitisation or a raised total IgE level and the eosinophil count is more than 0.5 x 109 per litre.
If there is still doubt about the diagnosis, refer to a paediatric specialist for a second opinion, including consideration of a bronchial challenge test.
Consider asthma in a child over 5 years if:
If the child is unable to perform objective testing
- Continue to treat based on observation and clinical judgement
- Try doing tests again every 6 to 12 months until satisfactory results obtained
- Consider referral to specialist if child repeatedly cannot perform objective tests and is not responding to treatment
When to diagnose asthma in children and young people aged 5 to 16 years
PDF: Objective tests for asthma in children and young people ages 5 to 16 years.
Code asthma after demonstrating any objective variability and a response to treatment.
Occasionally, symptoms subside independently, unrelated to the use of ICS. If no significant improvement is observed, cautiously discontinuing the ICS and advising parents to monitor the situation could be considered. Should symptoms reappear, instruct the parent to restart the ICS and inform you. If symptoms remain absent upon restarting, advise close monitoring by the parent, prompting them to report any recurrence. Providing parents with a peak flow meter for home use can aid in capturing variability during symptomatic periods.
FeNO testing and Spirometry may not be available in all areas of West Yorkshire. If there is clear peak flow variability and a response to treatment, this may suffice.
Do not rule out other diagnoses if symptom control continues to remain poor after treatment.
Review the diagnosis after 6 weeks by repeating any abnormal tests and reviewing symptoms.
Further information
Making the diagnosis of asthma in Children video presented by Dr Katharine Hickman, GP respiratory lead for West Yorkshire.
e-learning for healthcare: children and young people's asthma
New BTS/NICE/SIGN asthma guideline 2024
References
Global Initiative for Asthma: Global Strategy for Asthma Management and Prevention, 2023
Asthma: diagnosis, monitoring and chronic asthma management (BTS, NICE, SIGN) NG245, 2024