Tics are sudden, rapid and repeated body movements or sounds that serve no purpose. They are involuntary meaning your child is not doing them by choice.
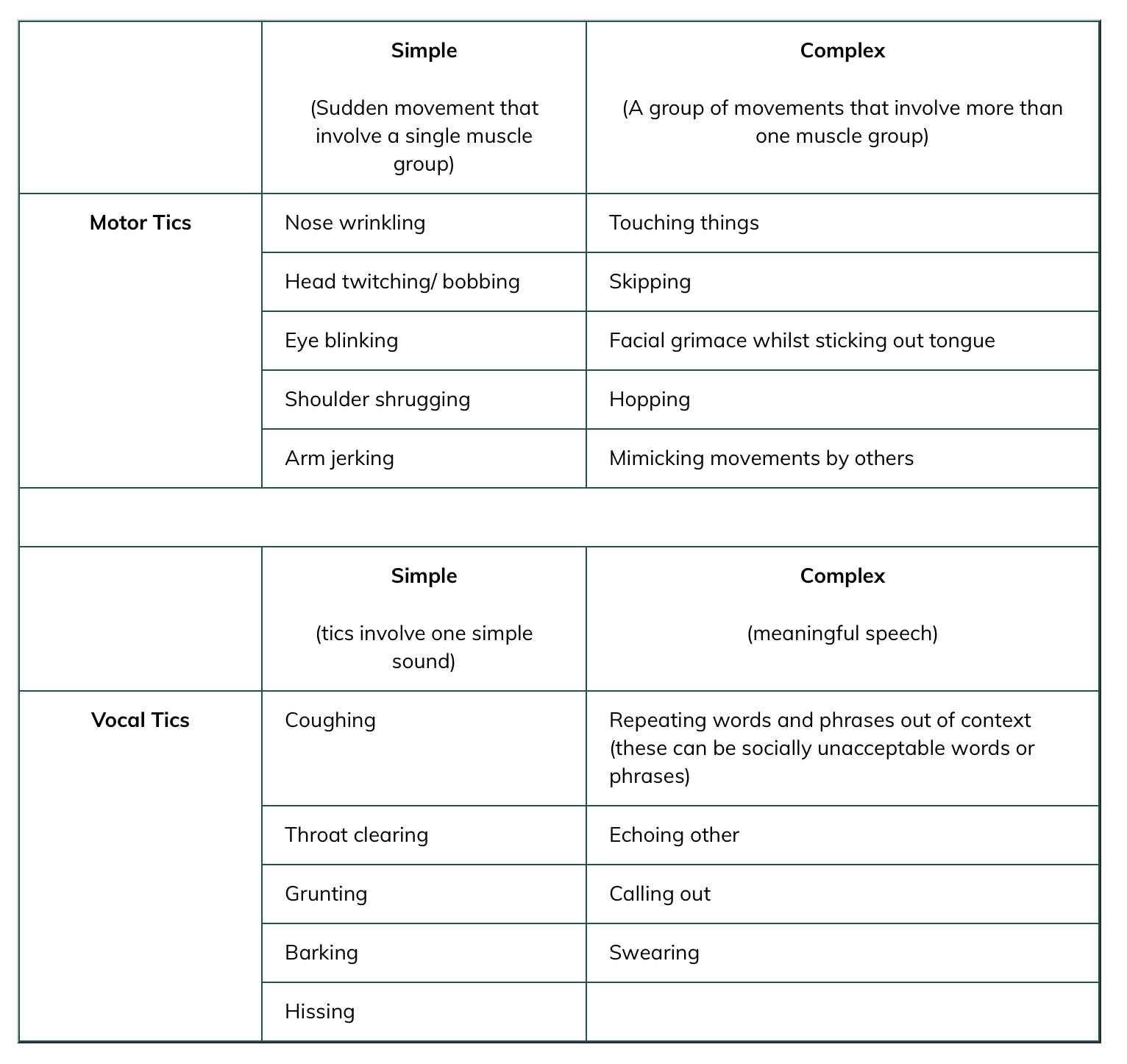
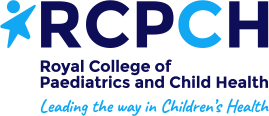
The movements (called motor tics) can affect any part of the body although most often affect the head and neck. Common examples of motor tics include rapid blinking, twitches in the neck and nose wrinkling.
The sounds (called vocal tics) commonly involve sniffing, tutting or throat clearing noises.
Tics can be simple. This means they involve just one muscle or making a noise.
Tics can also be complex. Complex tics involve lots of muscles moving together or spoken words, for example jumping on the spot or repeating words.
Some tics can be hard to spot whereas others can be very noticeable to other people.
Although tics vary from person to person, they often share certain traits.
When do tics happen?
You may be able to predict when your child will have tics. Some children have lots of tics when watching TV or playing video games. Other children will experience more tics at home than at school. Although these situations are different from child to child most families can pick out the context in which their child is most likely to tic.
Children and young people often get a ‘premonitory urge’. This is an odd or unpleasant sensation that builds up until the child tics. The tic relieves the sensation. Some children describe this as a sense of pressure or like the feeling they get if they need to scratch an itch. Other children find it very difficult to describe.
Although tics are involuntary in the sense that people do not choose to do them, they often are able to suppress or ‘hold in’ a tic if they feel they need to. This does not stop the urge building up and children often find it hard to supress a tic for long period of time.
It can be hard to describe what it feels like to have a tic. Try the following exercise:
Try to not blink, for as long as you can. The longer you don’t blink, the more you want to blink. This is what it feels like to have an urge to tic.
Examples of tics:





 I Tic by Abby Hargrove (Recommended 6 yrs +)
I Tic by Abby Hargrove (Recommended 6 yrs +) Can I tell you about Tourette syndrome? by Mal Leicester (recommended 9 yrs +)
Can I tell you about Tourette syndrome? by Mal Leicester (recommended 9 yrs +) The Tourette’s Survival Kit by Tara Murphy and Damon Millar (15 yrs +)
The Tourette’s Survival Kit by Tara Murphy and Damon Millar (15 yrs +)  Nix your tics by B. Duncan McKinlay (15 yrs +)
Nix your tics by B. Duncan McKinlay (15 yrs +) Welcome to Biscuit Land: A Year in the Life of Touretteshero by Jessica Thom (adults)
Welcome to Biscuit Land: A Year in the Life of Touretteshero by Jessica Thom (adults) Coping with Tourette Syndrome: A Workbook for Kids with Tic Disorders by Sandra Buffolano (workbook, 10 yrs +)
Coping with Tourette Syndrome: A Workbook for Kids with Tic Disorders by Sandra Buffolano (workbook, 10 yrs +) Tic Disorders: A Guide for Parents and Professionals by Uttom Chowdhury and Tara Murphy
Tic Disorders: A Guide for Parents and Professionals by Uttom Chowdhury and Tara Murphy A Family's Guide to Tourette Syndrome be John T Walkup, Mink, Black et al
A Family's Guide to Tourette Syndrome be John T Walkup, Mink, Black et al