Vulvovaginitis
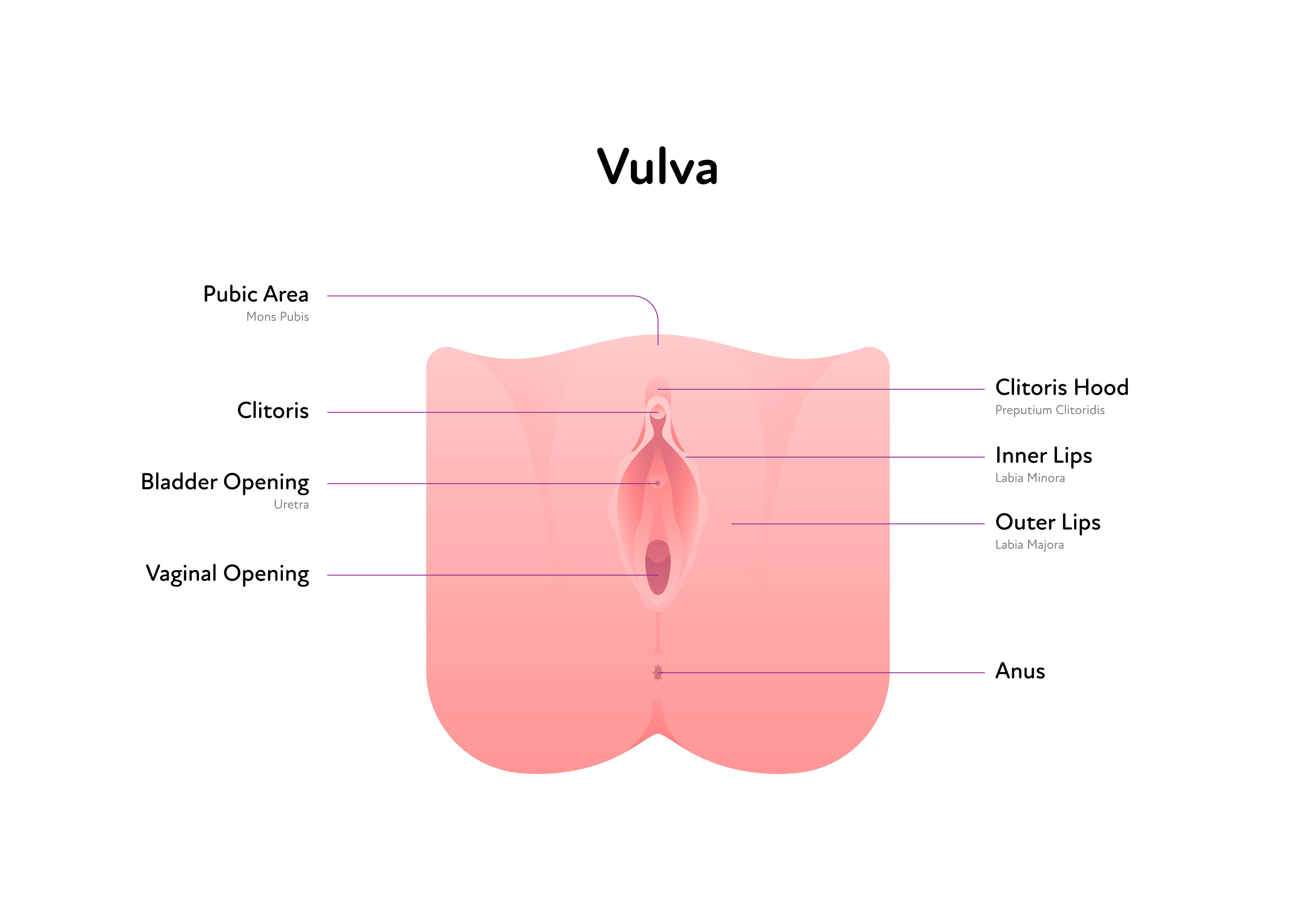
Vulvovaginitis is inflammation or irritation of the vagina and vulva (the outer part of a girl's genitalia).
Mild vulvovaginitis is common in young girls, especially between the ages of 2 to 7 years. It will affect most girls at some stage. Vulvovaginitis tends to improve as your child gets older and approaches puberty.
Signs and Symptoms
- Itchy and sore in the vaginal area
- Some discharge from the vagina which may be white, green or yellow and can be smelly
- Redness of the skin between the labia majora (outside lips of the vulva)
- Burning or stinging which can be worse when they do a wee (because the skin is sore)
In most cases vulvovaginitis is not a serious problem. Specific medical treatment and tests are usually not needed. It should improve with the simple steps below.
Causes of vulvovaginitis
- Before puberty the skin of the vagina and vulva is thin and less resistant to infection. The labia (lips) are flat and underdeveloped so do not protect the area well
- The vagina does not become acidic until after puberty. This acidity protects against infection
- The vagina and vulva are very close to the anus. This means bugs from your child's bottom can easily irritate the area. Young girls are still learning about keeping clean and wiping from front to back
- Moisture and dampness, especially in the first few years after potty training
- Bubble bath, soap and antiseptics can cause irritation
- Threadworms
Treatment
Treatment aims to protect the sensitive vulval skin from irritation.
Use a moisturiser to protect the skin
- Use a fragrance free moisturiser such as Hydromol, Epaderm or Cetraben cream
- You may find Cetraben or Hydromol ointment stings less than cream if she is very sore
- Apply (don't rub) the cream or ointment onto the outer and inner lips at least twice a day to soothe and protect the skin
- Continue to use even when she does not have symptoms to protect the skin and prevent flare ups
- Washing with only water can cause dry skin and make itching worse. Use a fragrance free moisturising cream as a soap substitute to clean the vulval area
- Apply the moisturiser before she gets in the bath or shower. Rinse it off and then reapply afterwards
- If it stings when she does a wee, you can apply the cream or ointment beforehand to protect the skin. Put some cream on the toilet paper to wipe afterwards
- Ideally underwear should be washed with non biological washing liquid rather than powder.
Avoid irritants
- Avoid fabric conditioners and biological washing powders
- Encourage a shower immediately after swimming to wash off the chlorine. Some girls find it helpful to use a moisturiser just before swimming to protect the vulval skin
- Avoid using soap, shower gel, shampoo, scrubs, bubble bath and baby wipes in the vulval area
- Never use feminine hygiene products or wipes
- Do not shampoo her hair whilst she is still sat in the bath. Shampoo in the bath water can be irritating
- Try not to clean the vulval area more than once a day. Over cleaning can worsen symptoms
- Avoid using sponges or flannels to wash the vulva
- Gently pat the vulva dry with a soft towel after bathing
- Teach her to wipe from front to back after going to the toilet
- Make sure her bottom is clean after doing a poo
Encourage air
- Wear loose cotton underwear. Try buying underwear a couple of sizes too big
- Avoid tight clothes such as tights, leggings and tight jeans
- Encourage her to sleep without underwear
Treat threadworms
If your daughter also has an itchy bottom or you have seen threadworms then this needs treatment. You can buy the treatment for threadworms from your local community pharmacy.
Contact your GP if:
- Symptoms are not improving despite the above treatment. If she is very sore the GP may do a skin swab but be aware the results are not always helpful.
- She wakes at night with vulval pain
- You notice any blood in the discharge
- Your child has a fever, abdominal pain or is passing urine more frequently than normal. Your GP may want to check that she does not have a urine infection.
Help your daughter stay safe
As your daughter has a genital problem the doctor or nurse may need to examine her. This can be a good opportunity for parents and carers to talk with their daughters about staying safe. The NSPCC offer an excellent online resource for this called talk Pants.