Functional Symptoms
Functional Symptoms is a term used to describe physical symptoms with no apparent biological cause.
When symptoms seem to be caused by problems in the nervous system, but you do not have a specific neurological condition, doctors may refer to your symptoms as Functional Neurological Symptoms.
Just because symptoms have no obvious biological cause, it does not mean the symptoms are imagined or not real.
So, sometimes, pain sticks around longer than it needs to and sometimes there is no actual injury or problem causing the pain, but it is still definitely real. The usual medical treatment of pain relief does not work very well for this kind of pain. When this happens, the brain seems to be confused, sending pain messages when it doesn’t need to.
Functional Symptoms can be frustrating because:
- The medical tests for your symptoms are all normal, but symptoms still occur.
- It can be hard to understand a diagnosis of Functional Symptoms.
- It can feel as though other people think your symptoms are imaginary.
However, you are not alone! Functional symptoms are common, with one in ten adolescents experiencing them! These symptoms account for up to 45% of all GP appointments, and half of all new visits to hospital clinics in the UK.
The aim of this pack is to educate and provide support for those experiencing Functional Symptoms.
🖨 Printable version of this resource pack
This pack has been produced with Frimley Health NHS Trust in partnership with Healthier Together.
Common functional symptoms:
- Abdominal pain
- Pain in the muscles or joints
- Tiredness
- Chest pain
- Heart palpitations
Common functional neurological symptoms:
- Tingling in the hands or feet
- A tremor in one or both arms
- Headaches or migraines
- Changes in eyesight like blurred vision or seeing flashing lights
- Movement difficulties (abnormal movement or positioning of part of the body). Specific movement difficulties can include arms or legs shaking uncontrollably, jerky types of movements, spasms, and gait (walking) problems
- Collapsing and fainting are also common functional neurological symptoms
The mind-body link: The computer analogy
There are several ways of describing the link between the mind and body which can help us to understand Functional Symptoms. Let’s start with a Computer Analogy.
Terminology
-
Hardware: the collection of physical parts of a computer system. For example, the monitor, keyboard, and mouse. The hardware is comparable to the brain.
-
Software: the programme, or instructions, that tell the hardware what to do. The software is comparable to the mind.
Think of the brain and nerves as a computer that sits on a desk. But the electrical messages that run through the nervous system are like the computer’s software. When the computer breaks, sometimes things go clearly wrong with the hardware (you can see the part is physically damaged, it can be fixed and replaced). However, sometimes things go wrong with the software. Whilst we cannot see these changes, sometimes reprogramming the software can help make positive change towards fixing the computer.
The same can be said of Functional Symptoms. Sometimes the brain picks up messages that something is wrong, and we can experience symptoms because of this. However, we cannot see anything physically wrong in medical tests, such as scans or blood tests (there is nothing wrong with the hardware, and therefore it cannot be replaced or fixed). Software problems may include psychological and social components, and therefore some of our ‘reprogramming’ needs to include these elements.
The mind-body link: How does it work
We can explain Functional Symptoms by talking about common examples of the link between psychology and biology.
Functional Symptoms are not all in the mind, but neither are they all in the body. To understand them we have to think about how the mind and body work together. Our body and mind work together and affect each other.
-
Scientists tell us that our brain communicates with our body, and our body communicates with our brain. Messages travel down the nerves from the brain to the body, and back again from the body to the brain.
-
Hormones are natural chemicals that travel the body through the bloodstream. Some hormones are produced in the brain and affect the body. Some are made in the body and affect our brain, which has an impact on our feelings and emotions.
Everyday thoughts, feelings, and stressors play a part in making changes in our bodies.
Fear and Extraordinary Strength
In 1982 Angela Cavallo lifted a car off of her son, who was trapped beneath it. He had been fixing the underneath of the car when the tool holding it off of the ground broke. Seeing this accident made Angela fear for her son’s life. She was an average sized woman, but still managed to hold up the 3,000 pound vehicle for five minutes whilst the neighbours rescued her son from beneath it. This seemingly superhuman strength is a part of the ‘Fight vs. Flight’ response. The release of adrenaline during the Fight vs. Flight response encouraged blood to rush to all of her working muscles, meaning muscles can contract with more force and power than normal. It is possible that during situations of extreme psychological stress and/or danger, that the adrenaline rush enables us to unlock a muscle’s true potential that might otherwise not be achieved voluntarily.
This example shows the interaction between an extreme psychological state, fear, and our biology; demonstrating the Mind-Body Link.
The mind-body link: Examples
There are also many more common day to day examples of the Mind-Body Link.
Blushing
When you feel embarrassed, or shy, you may notice your cheeks going pink, this is blushing. Blushing is a physiological response to feeling shy or embarrassed.
Butterflies
Feeling worried or scared can sometimes give you the feeling that there are lots of butterflies fluttering in your tummy. For example, on your first day of your new secondary school you may feel butterflies in your tummy because you are worried or scared, but these go away once you feel more relaxed and comfortable.
Throat Lumps
You may notice that when you feel upset or anxious your throat may feel as though there is a big lump in your throat. Although your throat might feel tight, there is not actually anything blocking it. This is the bodies physical response to psychological distress. However, when your level of anxiety or upset lowers, the lump disappears.
Tears
Tears are a physiological response to emotions such as sadness, happiness, and anger, we cry when we feel strong emotions. This is an example of your body (hardware) and mind (software) interacting.
Stress
Walking into an exam can be very stressful. You may notice that your heart race increases as you walk into the exam room. Stress generated in the brain results in bodily changes, such as an increased heart rate. The mind influences the body.
Exercise and Mental Health
Physical activity causes the release of chemicals in our brains, such as endorphins, which improves our mood and makes us feel good.
The connections between thoughts, feelings, and behaviours
Some people experiencing Functional Symptoms can get caught in an unhelpful cycle. It is important to recognise what this cycle is so we can break it to improve quality of life.
Tips: For younger children exploring their emotions using this model, try using a smiley face system.
Fight vs. flight for younger children
The Fight vs. Flight Response is a good example of how psychological distress can affect our physical symptoms! Anxiety is an excellent example of a psychological state which can contribute towards Functional Symptoms.
Thousands of years ago, when we were cavemen, stress and anxiety were very useful emotions because they helped us act in the face of immediate danger, keeping ourselves safe. For example:
A bear jumps out in front of you > you feel anxious > physical changes occur in your body, preparing you to either fight or run away > you fight or run away > you are now safe and your anxiety is relieved > your body returns to normal.
Anxiety is not always as helpful in today’s environment. Our body still reacts in the same way as it did thousands of years ago, however, the world today is much more complicated and many of the things that make us worry cannot be fixed immediately. This can leave us with feelings of anxiety, which are difficult to resolve instantly.
However, anxiety exists for a reason, and can be helpful in protecting us from immediate danger.
When you feel anxious you may notice several changes in your body. Circle the signals you notice when you get anxious:
Tip: When your child is in fight vs. flight, help them to focus on regulating their breathing. Avoid using phrases such as calm down, instead use let's breathe or in through the nose, out through the mouth or you're okay, just breathe.
Changing how you cope with symptoms: Doing too much or too little
Pacing is a skill which enables you to consistently carry out activities without causing excessive tiredness or inactivity. Pacing is the middle ground between doing nothing and doing too much. Over time you may notice that pacing enables you to do more.
-
Choose an activity, such as seeing your friends or school work.
-
Measure the length of time you feel physically and emotionally comfortable doing this. Do this at least 3 separate times on good and bad days.
-
Take the average of these times. This helps you find your comfortable starting point (amount of time) to spend on these activities. Try to stick to this time, no more and no less.
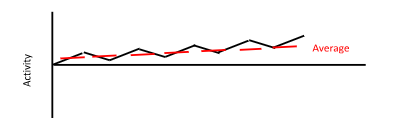
Remember:
-
Pacing can give you more control.
-
Pacing is about judging when to stop an activity based on time and not mood.
-
The comfortable starting point should be used on both good, and bad days. It is normal to find it difficult to limit yourself on good days.
-
Using a comfortable starting point leads to improved tolerance and achievement.
Changing behaviour and enjoying yourself
When we experience Functional Symptoms, we can often stop doing things that we used to enjoy. However, avoiding things often makes us feel worse in the long term.
-
The first step is to think about things you have stopped doing, are doing less, or are avoiding as a result of your symptoms. Make a note below of things you are avoiding because of how you are feeling.
|
Things around the home
|
|
|
Things at work or school
|
|
|
Hobbies or interests
|
|
|
Social activities with friends and family
|
|
|
Anything else
|
-
Once you have filled in Section 1, the next step is to plan how easy it would be to start doing some of the avoided activities again. It may seem overwhelming in the beginning, however, it is much easier if you break the process down into smaller steps.
-
Create a ladder (hierarchy) of things you avoid with the ones you are most anxious about at the top, and the ones that bother you less at the bottom. Try to include a good mix of the things you wrote down in Section 1. Start to tackle your symptoms and the things you avoid by starting at the bottom of the ladder and gradually working your way through each step. Before completing each task, write down what you think will happen, and follow this up by writing down what happened after task completion. Hopefully, you will start to see that it is mostly not as bad as you think it is going to be.
Turn your phone landscape to view this table in full.
 |
Situation |
Difficulty – 0 to 10 |
|
Example: playing rugby again |
10 (most difficult) |
|
|
Example: texting a friend |
0 (least difficult) |
Here is a printable version of this exercise.
SMART goals
Having Functional Symptoms can cause you to stop taking part in activities you enjoy. Goal setting is about working out what you would like to be able to do, and working towards achieving it. Goal setting is a powerful way of improving your quality of life and sense of control. It is important that goals are meaningful to you and feel good.
A goal is something that you are motivated to work towards and achieve. When you are working on activity levels, it is important to set goals that can help to both motivate you, as well as direct your efforts and energy.
-
Specific: clearly state what you would like to happen
-
Measurable: will you be able to say it was achieved?
-
Achievable: are you able to complete the task independently?
-
Realistic: are you going to do it?
-
Timely: think whether it is ‘the right time’ to do this. Set yourself a realistic time limit to achieve this goal.
Specific
To create a specific goal it must answer the 6 ‘W’s.
-
WHO is this goal for/who is involved in it?
-
WHAT is it that needs to be accomplished?
-
WHERE should this goal take place?
-
WHEN will this goal be completed, or how long will it take?
-
WHICH things or requirements, and constraints, need to be identified?
-
WHY does this goal need to be accomplished? What is its purpose?
For example:
‘I want to use Progressive Muscle Relaxation to help manage my pain’ as a SMART goal would be:
‘I want to use Progressive Muscle Relaxation 30 minutes, everyday at home for one month, to reduce my symptom severity’.
Measurable
Measurable goals make it easier to stay on track to meeting your goals. Questions like ‘how much’, or ‘how many’, or ‘how will I tell if I met my goal’ is a good way to determine what to measure. For example, practicing Progressive Muscle Relaxation for 30 minutes everyday is quantifiable and measurable. You can track your progress and see results.
Realistic
When you are coping with functional symptoms you need to have goals which are realistic and reasonable. It is easy to get ahead of yourself. Sometimes people fall into the trap of getting overwhelmed by goals which seem impossible. Make a realistic goal by breaking into smaller goals.
Timely
An important factor in achieving your goals is seeing the progress you have made. Set a time limit to complete your goal. For example, practice progressive muscle relaxation for 30 minutes each day, for a month before you tackle another goal. Write down your progress, seeing progress can motivate and encourage you.
Doing more
Mood can be greatly affected by what we do, when we do it, and with whom.
Keep track of what you do each day and make sure you are spending your time doing enough things that give you a sense of:
-
A - achievement
-
C – closeness to others
-
E – enjoyment
Being mindful of these 3 things when goal setting may help you to set meaningful SMART goals. Doing more also allows less time for negative and unhelpful thoughts and overthinking, which will have a positive effect on mood.
Improving sleep
Sleep difficulties are very common in individuals with Functional Symptoms. It is important to develop positive sleeping behaviors to help reduce anxiety and symptoms severity.
Routine
-
Sleep at regular times each night, this programs the brain and internal body clock to get used to a set routine.
-
It is important to try and wake up around the same time each day. If you have a bad night, still try to wake up at the same time in the morning. Catching up on sleep on a regular basis can disturb your sleep routine.
-
The amount of sleep you need changes as you grow.
Preparing Your Room
-
Make your bedroom just for sleep, try to avoid eating your meals in bed, or playing games in bed. Your bed should be for sleeping only.
-
Keep your bedroom tidy and free of distractions at bedtime. Clear away any toys or clothes lying around.
-
Keep the room at a good temperature and try to reduce light. Keeping light levels dim encourages the body to produce the sleep hormone, melatonin. If you are worried about the dark, you could try having a small night light.
Wind Down Before Bed
-
Having a warm bath can help your body to reach a temperature that is ideal for rest.
-
Avoid using smartphones, tablets, or other electronical devices for roughly an hour before bed. The light from the screens of these devices may have a negative effect on sleep.
-
Relaxation exercises, such as light yoga stretches and those included later in this pack can help to relax the muscles. However, vigorous exercise will have the opposite effect.
-
If your mind is busy, write a to-do list for tomorrow or write down your thoughts. This will help to organize your thoughts and clear your mind of any distractions.
Supporting children and teenagers experiencing functional symptoms
It can be difficult to see your child or teenage struggling. However, as an adult there are ways in which you can help improve their ability to cope with functional symptoms:
Reassurance. Although we do not know the exact organic cause of functional symptoms, your doctor will have completed tests to check that there are no other concerns. It is important to reassure your child that although their symptoms are real (and you understand that they are not making them up), they are not dangerous.
Record. When you first notice symptoms, you may like to keep a symptom diary. This may be helpful to learn about triggers and factors that make the symptoms better or worse. Please ask your doctor for a symptom diary if you plan to see them again, and they think that this would be helpful.
Distract and reduce focus on functional symptoms. It can be difficult to know how to respond to a child or young adult who is struggling. Often, the natural urge is to pay attention to signs that they may be suffering and to reassure them. It is important to avoid making the child or young person worry or become anxious, as they may focus on their symptoms more. Although it is challenging as a parent, it is important to minimise attention on the symptoms, for example, by not asking how the symptoms are. When their functional symptoms start, you may find it more beneficial to help the young person focus on something other than their symtoms, perhaps by engaging them in something they enjoy.
Encourage normal activities. It is important to not stop the young person doing the things they enjoy due to a fear of functional symptoms. You can reinforce ‘well behaviour’ (for example doing enjoyable activities) and give them confidence to resume their hobbies and interests, despite their symptoms.
Provide encouragement. Children and young people will feel more confident in their ability to cope with their symptoms with your support and confidence. Your role is to provide positive encouragement that they can cope with and manage their symptoms.
Support. Functional symptoms may affect your child or teenager’s ability to complete homework, coursework, and revision. Offering support with studies may relieve some of the stress, in turn decreasing the chance of reoccurring symptoms. You may like to provide this information to their school or college so they can provide extra support where necessary.
Guided self help worksheets
Calming The Body
Feeling relaxed can help reduce symptom severity.
Progressive Muscle Relaxation (PMR)
Muscle tension is commonly associated with stress and anxiety, it is the body’s natural response to potentially dangerous situations. Even when there is no danger, our bodies can still respond in the same way. You may not always realise that your muscles are tense, it may be as subtle as your jaw clenching, or as obvious as your shoulders feeling tight and hunched. PMR is a deep relaxation technique which is based upon the simple practice of tensing one muscle group at a time . This is followed by a relaxation phase with release of tension. This is very useful before bedtime.
During deep breathing your blood is oxygenated, triggering the release of endorphins, whilst also decreasing the release of stress hormones, and slowing down your heart rate.
Calming The Mind
Strategies for managing the anxiety and stress that is often associated with functional symptoms.
Worry Trees are helpful in reducing levels of anxiety surrounding both hypothetical situations and current problems.
Help yourself to feel more relaxed by thinking about things that make you feel calm and rested. For example, picturing your favourite place. This can be either independent, or you can take a guided visualisation approach. A guided visual imagery relaxation task has been provided in this pack.
A powerful stress reduction and relaxation tool, that can be applied at any time, in any location.
This is a useful technique for remaining grounded in the present, to alleviate symptoms of stress and anxiety.
These are phrases that you can say to yourself that are supportive. For example “Just because it has happened before it does not mean it will happen again”
Online resources
Apps:
Smiling Mind Mindfulness and Sleep
Calm Meditation and Sleep
Headspace Meditation
Think Pacifica Progressive Muscle Relaxation
Other pain resources:
Pain Concern
The Pain Toolkit. This source lists a collection of useful resources for healthcare professionals, families of, and people living in pain
- The Retrain Pain Foundation has a good selection of short videos that are helpful in understanding pain
Great Ormond Street NHS Foundation Trust provides information on chronic pain
Other useful websites:
-
Functional Neurological Disorder (FND) : a patient's guide. This website has been compiled by neurologists and gives detailed information about neurological symptoms (such as weakness, numbness or blackouts) which are not due to neurological disease
-
Non-Epileptic Attacks. This website is compiled by health professionals for patients. It gives information about attacks which look similar to epileptic seizures, but which are not due to the abnormal electrical activity in the brain that causes epilepsy
 Resources for Teachers, Parents, Carers, and Children. Don't want to talk? Text YM to 85258, the Young Minds Crisis Messenger for free 24 hours a day, 7 days a week support.
Resources for Teachers, Parents, Carers, and Children. Don't want to talk? Text YM to 85258, the Young Minds Crisis Messenger for free 24 hours a day, 7 days a week support.  Kooth is a free, safe, and anonymous online wellbeing community for young people. You can sign up without being referred by anyone and you don’t need to download any apps.
Kooth is a free, safe, and anonymous online wellbeing community for young people. You can sign up without being referred by anyone and you don’t need to download any apps.- Moodcafe.co.uk Stress and Anxiety
- Anxiety and Depression
- Getselfhelp.co.uk Mindful Activity
- Getselfhelp.co.uk Relaxing Imagery
- Getselfhelp.co.uk Thought Distancing
- Getselfhelp.co.uk Supporting Sleep
Local resources
West Yorkshire
West Yorkshire Night OWLS is available 8pm to 8am every day for children, young people, parents and carers across West Yorkshire. Call free on 0800 1488 244 or text on 07984 392700. Visit the website to use the online chat function www.wynightowls.org.uk
Kooth is an online counselling and emotional well being platform for children and young people. 10 to 18 year olds can chat one to one with counsellors, access self help articles and connect with peers through live moderated forums.
Bradford and Craven
Healthy Minds for young people is there to help you find support, information and advice if you are struggling with how you are feeling and thinking.
Wellbeing hubs provide support and free specialist advice on a number of areas including mental health. If you are under 16 you need to bring a parent or carer with you.
Leeds
MindMate was designed with young people to provide information about common mental health issues and where to find support.
Kirklees and Calderdale
Open Minds provides advice, information, support and signposting to local and national emotional health and wellbeing services.
Wakefield
WF I Can is an online resource for young people in Wakefield where you can find information and advice.